Introduction: Disparities in cancer care are widely reported with the reasons being multifactorial. Delays in referral and distance to travel along with lack of public transportation are common structural barriers that further exacerbate the racial and income related disparities in the care of hematological malignancies. A lower proportion of black patients receive transplants, both autologous (AutoSCT) and allogeneic (AlloSCT) for similar indications as compared to white populations. Racial disparities are evident in transplant utilization for hematologic malignancies. When offered similar therapy, the outcomes might be better in black patients as compared to White populations underscoring the effect of biology of the disease. South Georgia region has a very high poverty rate with many counties having a median income much less than the national average. We report our efforts to increase access for hematological malignancies for patients in predominantly rural and minority focused settings.
Methods: We reviewed charts of all patients referred to our center from 01/2014 to 12/2022. We divided patients into three groups. Cohort A. 36 months from 1/14 to 06/2017. Cohort B, 36 months from 07/19 to 12/22. The intervening two years were utilized for outreach development. Physicians visited all the community centers and created an easy access physician to physician referral system. In addition, in partnership with community oncology, two clinics were established at 65 miles and 89 miles to our center. Referrals from these sites were seen at these outreach clinics. The total number of Auto and Allo SCT and clinical trial enrollment data were obtained from databases. Outcomes data is from that reported on the SCT patients to the national databases. Statistics are descriptive.
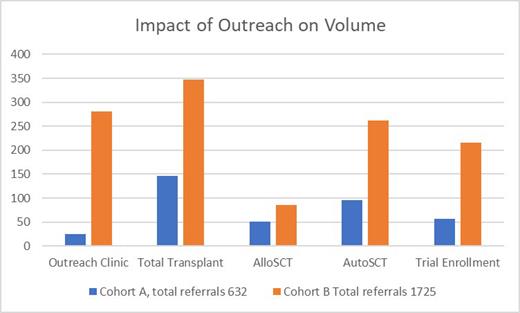
Results: Post outreach activity showed a significant increase in volumes. (Figure 1) Patients' referrals for heme-malignancies were up to 1725 compared to 632 (170% increase). The median distance travelled in these groups was 52.7 vs 17.8 miles (range 0-525 vs 2342) demonstrating the larger area covered from outreach activity. Considering our metro area radius of 20 miles, 62% of patients were outside our immediate area. Excluding the patients withing the 20-mile radius between the two groups, median distance travelled by patients in cohort B being 99 miles vs 60 miles in cohort A. The increase was consistent across all races. There was an increase from 254 to 588 in black population and 355 to 1028 in the white populations. The outreach clinics set up in partnership with the community practices added a significant new patient population with numbers increasing from under 25 in the initial cohort to above 250 in cohort B. Overall this increase translated to higher number of transplants with 146 transplants in cohort A compared to 347 in cohort B, a 137% increase. The alloSCT increased from 51 to 85 and autoSCT from 95 to 262 between the two cohorts respectively. In addition, the addition of CAR-T further expanded the cellular therapy program with a total of 131 cellular therapy products in fiscal year 2023 compared to 39 in fiscal year 2015, a 235% increase. Our outcomes have consistently improved as well with the most recent CIBMTR 1 year survival of 74% while the predicted was 68%. Similarly, the increase in referrals translated to an increase in clinical trial enrollment with the most recent 3-year period having an accrual of 216 as compared to 56, a 285% increase overall and 185% in black patients, compared to the initial 3 years. Age is another commonly noted factor that results in lower access to care. Our model resulted in a significant increase in elderly patients as well with > 60 years of age patients increasing from 326 to 1017 while those above 70 increased from 149 to 549 in the respective cohorts.
Conclusions: Our model is easily reproducible and shows a substantial increase in the number of referrals for hematological malignancies. The recent approvals of complex therapies like CAR-T and other T cell engaging therapies necessitate a close collaboration between academic and community practices. Similar models if developed at other academic centers can significantly reduce structural barriers and might improve outcomes further in all patient populations.
Disclosures
Kota:Kite: Honoraria; Pfizer: Honoraria; Incyte: Research Funding; Novartis: Honoraria. Keruakous:Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding; BMS: Membership on an entity's Board of Directors or advisory committees. Cortes:Novartis: Consultancy, Research Funding; Abbvie: Consultancy, Research Funding; Biopath Holdings: Consultancy, Current holder of stock options in a privately-held company, Membership on an entity's Board of Directors or advisory committees, Research Funding; Forma Therapuetic: Consultancy; Gilead: Consultancy; Takeda: Consultancy, Honoraria; Pfizer: Consultancy, Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal